Today we discussed a patient with polyarticular gout presenting with fever and multiple swollen joints.
Precipitants:
Drugs: HCTZ, other diuretics, ASA, pyrazinamine, allopurinol, cyclosporin, other
Foods: Alcohol (red wine), Red Meat, Cheeses
Diseases: Myeloproliferative disorders, hematologic malignancies, renal failure
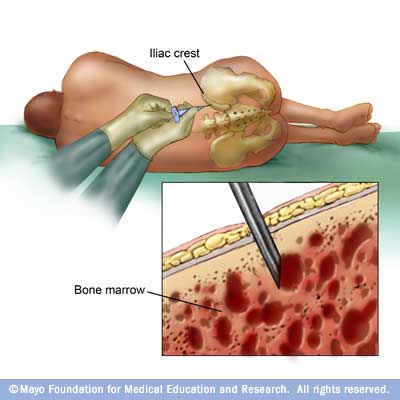
Diagnosis (how to do an arthrocentesis):
Synovial fluid cell count usually in the 10,000-20,000 range but can be as high as 100,000.
Crystals should be seen -- negatively birefringent needle shaped crystals which are intracellular
Acute
Treatment (usually one of):

NSAIDS: I.e. Naproxen 500mg PO BID
Steroids: Intrarticular (i.e. depomedrol 20-40mg) or systemic prednisone (i.e. 40mg x 3 days then taper by 10mg every three days)
Colchicine: colchicine 0.6mg po q1h x3 (diarrhea, nausea) then 0.6 OD-BID (renal dosed)
Long term Treatment:

Weight loss, avoidance of foods and drugs that precipitate
Initiate low dose colchicine if you are going to start anti-hyperuric medications to avoid precipitating an attack
Generally initiate therapy if one/more of: (i) urate nephropathy or recurrent stones (ii) destructive tophi (iii) greater than three attacks per year (iv) greater than 1100mg urinary urate per day
Some advocate for use of 24h urine urate -- if >800 then uricosuric therapy is contra-indicated. Titrate to uric acid less than 360umol/L
Uricosuric therapy:
Probenecid start 250mg BID titrate to 500-1000 BID
Consider vitamin C 500mg PO OD
Consider losartan as an antihypertensive if needed (has uricosuric effect)
Consider fenofibrate
Xanthine Oxidase Inhibition:
Allopurinol 100mg PO OD titrate to effect (usual dose ~ 300mg/day)
I have previously blogged about the approach to the mono/oligo arthritis (and septic arthritis) here.




 Weight loss, avoidance of foods and drugs that precipitate
Weight loss, avoidance of foods and drugs that precipitate